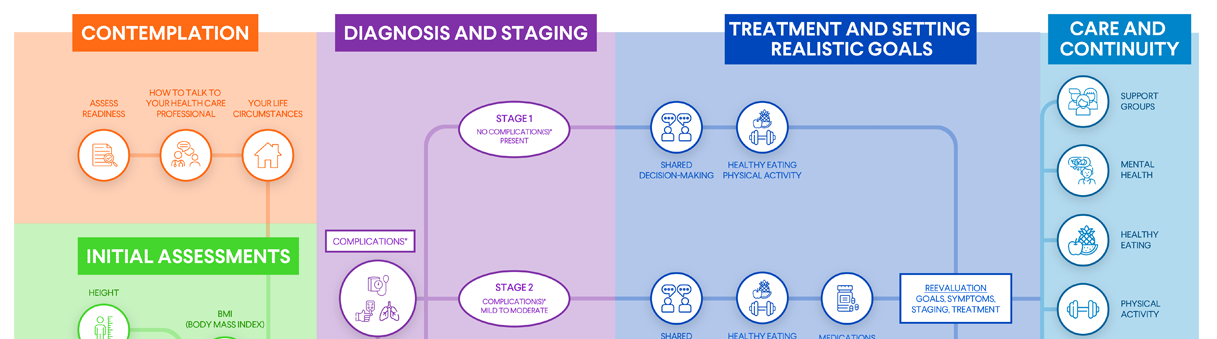
Treatment and Goals
Planning and Treatment, Stage 3

Planning and Treatment, Stage 3
Stage 3 obesity means you have at least one severe weight-related complication that requires significant weight loss for effective treatment. In other words, you have both obesity and one or more serious medical conditions that may affect your health.
The treatment goals for stage 3 obesity are to:
- Reduce your weight.
- Improve your weight-related health condition(s).
- Prevent other chronic health conditions from occurring in the future.
Managing your weight can also reduce your risk of developing obesity-related complications and many types of cancer, including breast cancer, colorectal cancer, and prostate cancer.
Stage 3 obesity treatment typically includes taking steps to reduce chronic disease risk and changing your behavior habits. Key treatment strategies are:
- Setting realistic weight management goals
- Healthy eating
- Physical activity
- Weight management medications
- Obesity surgery
Learn more about each treatment strategy below.
Setting Realistic Weight Management Goals
At the beginning of your obesity journey, try setting a modest goal — say, loss of 5%-10% of your body weight over the course of six months. This amount of weight loss has been shown to provide benefits in many obesity-related complications, including diabetes, high blood pressure, and non-alcoholic fatty liver disease. Once you meet that goal, you and your health care professional can set a new one.
Losing a lot of weight may require setting new goals multiple times. By working with your health care professional, you can establish realistic goals that will produce results and motivate you to succeed.
Healthy Eating
Eating a healthy diet that includes nutrient-rich foods in right-size portions is one of the best changes you can make for your weight and health.
Keep the following tips in mind as you think about healthy eating — and be sure to ask your health care professional for whatever guidance and support you need.
- What to eat: A healthy diet includes a wide range of nutritious foods, including fruits, vegetables, whole grains, lean meats, poultry, eggs, seafood, low-fat dairy, nuts, seeds, legumes, and healthy fats.
- What to avoid: A healthy diet limits highly processed foods; sugar-sweetened beverages; alcohol; and foods with added sugar, saturated fats, trans fats, or sodium.
- Portion control: No matter how healthy your diet is, you'll lose weight only if you eat the correct number of right-size portions. A good source of information about portion control is the U.S. Department of Agriculture's MyPlate Plan.
- Calorie control: For slow, steady weight loss, many health care professionals recommend reducing daily calorie intake by 500-750 calories. You and your health care professional can decide together how many calories you need each day. In a typical healthy eating plan, total daily calorie goals that include a reduction in calories for weight loss range from 1,200-1,600 for women and 1,500-1,800 for men. However, this varies for each person.
If you're currently following a calorie goal but not achieving any weight loss, you're taking in too many calories to lose weight. Your health care professional may recommend cutting your daily calories by an additional 100-200 calories. Your height, starting weight, and activity level all help determine what your daily calorie intake should be.
Meal plans to follow: Let your health care professional know if you'd like to follow a specific meal plan. Good options include the Mediterranean diet, the Dietary Approaches to Stop Hypertension (DASH) eating plan, and the MyPlate Plan.
Your health care professional may also recommend other types of eating plans, such as a low-carbohydrate or low-fat food plan, a low-calorie/high-volume food plan, a high-protein food plan, vegetarian eating, intermittent fasting, or a plan that substitutes some of your meals with meal-replacement drinks. Each of these plans has different pros and cons. Your health care professional can recommend the plan that's best for you.
A very-low-calorie diet is an option for some individuals, but it requires medical supervision and should be followed only if your health care professional recommends it.
Need extra support? Ask your health care professional to refer you to a registered dietitian or health educator.
Physical Activity
Increasing your physical activity burns calories and speeds up weight loss. It provides many other benefits, too, such as lower blood pressure, improved cholesterol levels, better heart health, stronger bones and muscles, better sleep, and improved mood. By getting moving, you help yourself in multiple ways.
Your health care professional will give you guidance on how much exercise you can do, what types of activities are best for you, and what types of exercise to avoid because of physical limitations or other factors.
Keep the following tips in mind as you think about physical activity — and be sure to ask your health care professional for whatever guidance and support you need.
- How much exercise to do: Any amount of exercise can benefit your health. But the general recommendation for physical activity is:
- 150 minutes per week of moderate-intensity physical activity (e.g., walking, swimming, biking, or playing tennis).
- Two days per week of muscle-strengthening activity that works all major muscle groups (i.e., legs, hips, back, abdomen, chest, shoulders, and arms). Strength training builds muscle mass, which contributes the most to metabolic rate. It's also very important for bone health.
- How to get started: It's fine to start with short bouts of activity and to increase duration over time. Start with something simple, such as walking a few minutes a day. As you become fitter, you'll be able to increase your walking distance and intensity. About 30 minutes a day, five days a week, is recommended. Alternatively, you could exercise for a longer duration on fewer days. Keep in mind that you can break up your activity into several shorter sessions throughout the day.
- Pick something you enjoy: You're more likely to stick with activities that you enjoy. No interest in jogging? No problem. Walk, hike, dance, play pickleball, or take a Zumba class instead.
- Work activity into your everyday life: Spending time with a friend? Go for a walk instead of a meal. Watching TV? Lift some weights while you watch. And your dog will love it if you start taking them out for extra walks.
- Track your progress: Using a step counter or other tracking tool may help you stay committed to exercise. The standard recommendation is 10,000 steps a day, but don't feel you have to start with that many steps. Begin with what feels doable, and gradually increase your daily step count goals over time.
- Join a gym — or not: Lots of people enjoy exercising at a gym, working out with a trainer, or participating in group exercise classes. But that doesn't mean you have to invest in a gym membership if you're not a fan of gyms. All you need to get started is a comfortable pair of shoes and a place to walk. You could also check out the many free exercise classes available online.
- Reduce sedentary behavior: Have a job that requires long hours of sitting? Try to schedule frequent breaks throughout the day to stretch or walk around, even if just for a couple of minutes.
Need extra support? Ask your health care professional to refer you to a physical therapist or medical exercise program.
Weight-Management Medications
Recommendations for weight management tend to focus on behavioral/lifestyle changes like healthy eating and physical activity. However, some people with obesity need something more.
If you have stage 2 or stage 3 obesity, your health care professional may bring up the possibility of taking prescription weight-management medications. Medicine cannot replace healthy eating and physical activity. But if you have certain weight-related chronic health conditions or have been unable to lose weight through other means, combining medicine with behavioral/lifestyle changes may help.
Consider this finding from the National Institutes of Diabetes and Digestive and Kidney Diseases (NIDDK): On average, after one year, people who combine prescription weight-management medications with lifestyle changes lose 3%-12% more of their starting body weight than people in a lifestyle program who do not take a medication.
Here's some information that can guide you in discussing weight-management medications with your health care professional.
How Weight-Management Medications Work
Weight-management medications come in both oral and injectable forms, but it's crucial to understand the correct dosage for each. The FDA has reported that overdoses can happen due to incorrect dosing, particularly with compounded medications. To ensure your safety, always consult your health care professional about the appropriate dosage for you.
Side Effects
Most medications cause side effects (unintended, often negative, reactions in your body). Side effects may be temporary or permanent. They may be minor or serious, or anywhere in between.
When studying medications, researchers keep track of the side effects that occur in people who take them. The common side effects must be included on the medication's package label.
It's important to ask your health care professional about the common side effects for any medications you're considering. Having this information can help you decide whether you want to take the medication and what to expect if you take it.
Common side effects of weight-management medications include:
- Headaches
- Nausea
- Abdominal pain
- Frequent bowel movements
- Constipation
- Diarrhea
- Dry eye
- Dry mouth
- Anxiety
- Depression
- Mood swings
- Dizziness
- Vomiting
- Increased heart rate
- Insomnia
Keep in mind that people respond to medications in different ways, so side effects can vary from person to person.
In addition, some medications may cause more serious side effects in people who have certain medical conditions or take certain other medications. Be completely open with your health care professional about your medical history and any medications or supplements you're taking. Your health care professional will let you know what kind of testing or monitoring you may need to watch for serious side effects.
If you take a weight-management medication and experience a side effect, tell your health care professional. Depending on the type and seriousness of the side effect, your health care professional may:
- Wait to see if the side effect lessens or stops.
- Recommend comfort measures or medications to help you cope (e.g., over-the-counter eyedrops for dry eye).
- Change your medication dose.
- Take you off the medication.
- Switch you to another medication.
Length of Treatment
As you and your health care professional discuss weight-management medications, be sure you understand how long you will stay on the medication. Some drugs should be taken only for a short time, while others are safe for longer periods of time. You should also understand whether you should expect to gain weight when you stop taking the medication.
Setting Realistic Expectations
Your health care professional can help you set realistic expectations about how much weight you may lose while taking a weight-management medication. Different drugs have different success rates, and people respond to drugs differently. Generally, people who take weight-management medications may expect to lose 5%-20% or more of their starting weight. But your results will depend on many factors, including starting weight, age, activity level, eating habits, stress levels, and sleep habits.
Medication Costs
Before choosing a weight-management medication, check with your health insurance carrier about your out-of-pocket costs.
FDA-Approved Medications for Adults With Obesity
The U.S. Food and Drug Administration (FDA) has approved five weight-management medications for long-term use. Please note: You won't find comprehensive lists of side effects for the medications below. Be sure to ask your health care professional about all side effects that could affect you.
- Phentermine/topiramate (Qsymia®): This is a capsule that decreases your appetite and helps you feel full after eating. Side effects may include headache; dizziness; trouble concentrating; tiredness; change in taste; a racing heart; and numbness or tingling in your arms, face, feet, and hands. It may not be taken with certain antidepressants or if you have glaucoma, an overactive thyroid, or certain heart or mental health conditions.
- Naltrexone/bupropion (Contrave®): This is a tablet that reduces your appetite to help you eat less. It's also used to help people stop smoking. People who have seizure disorders or take opioid medications should not take it. Since it can affect your heart, your health care professional will monitor your heart rate and blood pressure for the first 12 weeks. Side effects may include headache, dry mouth, constipation, nausea, vomiting, and, rarely, suicidal thinking.
- Liraglutide injection (Saxenda®): This medicine, injected once daily, reduces appetite and helps you feel fuller by slowing down stomach emptying. It's also prescribed to treat diabetes because it enhances your body's ability to produce insulin. Side effects may include nausea, vomiting, diarrhea, abdominal pain, constipation, injection-site rashes, and suicidal thinking.
- Semaglutide injection (Wegovy®): This drug has a similar mechanism of action as liraglutide but is injected once a week. It reduces your appetite and helps you feel fuller by slowing down stomach emptying. It's also prescribed to treat diabetes because it enhances your body's ability to produce insulin. Side effects may include nausea, vomiting, diarrhea, abdominal pain, heartburn, constipation, burping, suicidal thinking, and injection-site rashes.
- Orlistat (Xenical®, Alli®): Orlistat is a capsule that blocks the absorption of one-third of the fat in the foods you eat. It tends to be most effective for people who eat a high-fat diet. Side effects may include oily stools, stool leakage, loose stools, urgent bowel movements, stomach pain, gas, cramps, and irregular periods in women. Your health care professional may recommend vitamin supplements, because orlistat can reduce your body's ability to absorb certain nutrients from food.
- Tirzepatide (Zepbound™): Tirzepatide is a weekly injection that helps you eat less. It works by activating hormone receptors related to appetite. It has been approved by the FDA in adults with obesity or overweight and at least one weight-related health condition, such as type 2 diabetes, high blood pressure, or high cholesterol. Tirzepatide is also prescribed under the name Mounjaro® to help improve blood sugar in people with type 2 diabetes. Side effects may include nausea, diarrhea, vomiting, constipation, abdominal pain, indigestion, injection site reactions, fatigue, allergic reactions, belching, hair loss, and gastroesophageal reflux disease. Tirzepatide causes a type of thyroid tumor in rats, but researchers don’t know if it causes that type of tumor in humans.
Visit the FDA for more information about drug compounding.
Other Weight-Management Treatments
- Meal-replacement shakes replace meals with specially designed drinks.
- Pre-packaged meal replacement plans have specified amounts of calories and macronutrients. Meals can be purchased through various meal plans or can be made independently.
- Phentermine (Adipex®, Lomaira®, and Suprenza®) is an amphetamine-like pill that stimulates your central nervous system and decreases your appetite. It is only FDA-approved for a limited amount of time, depending on the state you live in (most common is three months or less).
Other promising weight-management therapies will become available in the future. For example, researchers are looking at medications that could bring about weight loss by altering gut hormones or gut bacteria. They're also investigating treatments that could change the action of certain genes related to obesity — a process known as gene editing.
Choosing the Right Medication for You
Once you and your health care professional have talked about your weight-management medication options, common side effects, and the results you can realistically expect to see, you can choose how to proceed. Don't feel pressured to make a quick decision — it's okay to take time to consider everything you and your health care professional have discussed.
Obesity Surgery
A healthy eating plan, physical activity, and behavior changes are crucial parts of any weight-management treatment plan. If you have stage 3 obesity, your health care professional may also talk with you about taking weight-management medications and/or having obesity surgery (also known as bariatric surgery).
Any type of obesity surgery is a major medical procedure. It requires considerable planning, recovery time, and lifestyle changes. That's why health care professionals recommend obesity surgery only when its potential benefits outweigh its possible risks.
There are several types of obesity surgery. Each has different pros and cons, and each helps with weight management in a different way. If your health care professional recommends obesity surgery, they will talk with you about which types of surgery might fit your needs. However, it's helpful for you to understand some basic facts about obesity surgery so you can make informed choices about it.
Here, we provide information to help guide you as you discuss your options with your health care professional.
Setting Expectations With Surgery
How much weight can you expect to lose if you have surgery? That depends on many factors, including the type of surgery, your starting weight before surgery, and the lifestyle changes you make afterwards.
On average, people who have obesity surgery lose 15%-30% of their starting body weight, according to NIDDK. Of course, results from surgery vary from person to person. In addition, you may regain your lost weight in the future if you don't stick with long-term lifestyle changes.
Your health care professional can help you set realistic expectations about how much weight you may lose if you have obesity surgery and its possible impact on your weight-related health conditions.
How Obesity Surgery Works
Obesity surgery works by making changes to your digestive system. For example, surgery may:
- Reduce the size of your stomach, which limits how much food you can comfortably eat.
- Change how your body absorbs nutrients from the food you eat.
- Limit the number of calories your body can absorb.
- Impact hunger and appetite hormones as well as the bacteria found in your gut.
Reasons to Consider Obesity Surgery
Losing weight as a result of obesity surgery could improve weight-related medical conditions such as type 2 diabetes, sleep apnea, high blood pressure, and unhealthy cholesterol levels. It could also reduce your risk of developing weight-related cancers.
Obesity surgery may even help lengthen life. For example, a 2018 study found that bariatric surgery extended life in study participants by 4.5 years compared with people of similar age, gender, and body mass index who did not have bariatric surgery.
Possible Risks of Obesity Surgery
Your health care professional will talk with you about the risks of surgery. Depending on the type of surgery, these may include:
- Side effects as a result of surgery: These include bleeding, scarring, infection, and blood clots. They can range from annoying to life threatening.
- Dumping syndrome: This condition occurs when food moves too quickly from your stomach to your intestines. This causes the release of excess hormones, such as insulin. It also allows excess movement of fluid into your intestines, which can result in symptoms such as flushing, rapid heart rate, abdominal pain, vomiting, and diarrhea. Dumping syndrome can usually be prevented by eating protein-based meals and avoiding simple carbohydrates.
- Gallstones: People who lose weight quickly after surgery have a higher risk of developing gallstones. These are deposits that form in the gallbladder and can cause intense pain.
- Ulcer: An ulcer is the erosion of tissue in the area where your stomach and intestines meet. It is usually treated with medication, but if it is severe, it may require surgical intervention.
- Stricture: This condition occurs when space in your stomach becomes too narrow to handle solid food. It can cause vomiting or nausea. Stricture requires a follow-up surgical procedure to open up the space in your stomach.
- Hernia: This condition occurs when part of your stomach, intestines, or other tissue pushes into a place it doesn't belong, usually in your abdomen. A hernia typically requires surgical repair.
- Additional procedures: About one-third of bariatric surgery patients require some type of follow-up procedure or hospitalization within five years of surgery.
- Nutrient deficiencies: After surgery, your body may not absorb nutrients as well. To protect your health, you'll need to take vitamin and mineral supplements for the rest of your life. If you don't get enough of certain nutrients, you may develop health problems related to nutrient deficiency, such as anemia (from a lack of iron) or osteoporosis (from a lack of vitamin D and calcium).
The Cost of Obesity Surgery
Obesity surgery can cost upwards of $15,000, depending on the type of surgery you have, postsurgical complications, and other factors, according to NIDDK. Some types of health insurance help pay for obesity surgery. For example, Medicare and Medicaid cover some surgery procedures if you have certain obesity-related conditions.
As you think about whether to have obesity surgery, ask your health insurance carrier about:
- What conditions you must meet to qualify for coverage
- How much of the cost of surgery would be covered
- What your out-of-pocket costs would be
Be sure you're well-informed so that you have no unexpected costs.
Preparing for Surgery
If you and your health care professional decide that obesity surgery is right for you, you'll receive detailed instructions about what to do before surgery. Steps may include:
- A physical exam. Your health care professional will look for medical conditions that can interfere with your surgery and recuperation.
- Education: There's much to learn about what to expect before, during, and after obesity surgery. Your health care professional may present this information in a class, a video, an information package, or some other means. As you learn about your surgery, make a list of any questions for your health care professional and be sure you receive the answers you need.
- Meeting with a dietitian: A dietitian is a health care professional who specializes in food and nutrition. They help you learn about different food types and work with you on setting personalized nutrition goals. They also instruct you on what type of eating plan to follow before and after surgery.
- Meeting with an exercise expert: Learn what physical activities you should do before and after surgery. Being physically active prior to surgery will decrease your risk of complications during and/or after surgery.
- Meeting with a mental health care provider: A psychological evaluation before surgery helps ensure that you are emotionally ready for the procedure. Be sure to tell your mental health care provider if you have a history of mental health conditions, disordered eating, or trauma that could be triggered by the surgery.
- Meeting with a behavioral health expert: You'll need to make many changes to your behavior habits with surgery. A behavioral health expert will help you learn what changes you'll need to make and how to successfully shift your behavior habits.
- Connecting with a support group: Your health care professional may recommend that you join an in-person or online support group for people who have had obesity surgery. A group can offer support, information, a sense of community, and an opportunity to share your experiences and learn from others who have had obesity surgery.
- Presurgical testing: Your health care professional will perform a blood pressure test and blood tests. They may also do lab work or imaging to check your vitamin and mineral levels, heart health, breathing, and more. They'll also ensure you're up to date on scheduled cancer screenings before surgery.
- Diabetes monitoring: If you have diabetes, your health care professional will check to see if your blood sugar is in good control before surgery. If it's not, they may recommend delaying surgery until your blood sugar is better controlled to decrease the risk of complications during and after surgery.
- Quitting smoking: If you smoke, you must quit for six weeks before surgery and ideally not start again. Your health care professional can refer you to stop-smoking resources to help you quit.
- Pregnancy counseling: If you may become pregnant, your health care professional will talk with you about birth control. Pregnancy is not recommended for 18 months after obesity surgery.
- Understanding what to do in the days and hours leading up to surgery: Your health care professional will let you know what to eat before surgery, when to stop eating, and other important details.
Types of Obesity Surgery Approved by the FDA
The U.S. Food and Drug Administration has approved the following types of surgery options for adults with obesity:
Laparoscopic Adjustable Gastric Band: Commonly known as adjustable gastric band surgery, this procedure places an inflatable silicone band around the top part of your stomach. The band creates a smaller stomach pouch with an adjustable opening. The small pouch limits the amount of food you can eat and helps you feel fuller faster after eating. If needed, the band can be adjusted. This type of surgery is reversible. It's less popular now than it once was because of potential complications and because it typically leads to less weight loss than other obesity surgery types.
Laparoscopic Sleeve Gastrectomy: Also known as gastric sleeve surgery or sleeve gastrectomy, this is a procedure where much of your stomach is removed. The remaining part of your stomach is a banana-shaped sleeve. Weight loss can occur because the new, smaller stomach holds less food. In addition, the portion of the stomach that's removed is where hunger hormones are produced. Patients who have sleeve gastrectomy tend to feel less hungry and get fuller faster. This procedure is not reversible.
Roux-en-Y Gastric Bypass: Commonly known as gastric bypass surgery, this procedure creates a small stomach pouch and connects it directly to your small intestine, bypassing the majority of your stomach and about 30% of your upper intestines. This new, smaller-sized stomach pouch restricts the amount of food you can eat. It also results in the absorption of fewer calories and nutrients from your food. Additionally, this shift changes the action of hormones and bacteria in your gut in a way that can reduce your appetite. The surgery can be performed laparoscopically, where instruments are introduced into your abdomen through small incisions. This eliminates the need for open abdominal surgery. Gastric bypass surgery is difficult to reverse.
Biliopancreatic Diversion With Duodenal Switch: Also known as "mixed surgery," this procedure is a combination of sleeve gastrectomy surgery and gastric bypass surgery. A sleeve gastrectomy is first performed, then the remaining portion of your stomach is attached to the lower one-third of your small intestine. As a result, the food you eat bypasses 70%-80% of your small intestine, which lowers the amount of calories and nutrients your body can absorb. Although this type of surgery leads to good results, its higher complication rate and risk of nutrient deficiency make it less popular than other types of surgery. It is partially reversible.
Endoscopic Sleeve Gastroplasty and Transoral Outlet Reduction: This procedure reduces the size of your stomach, which helps you eat less food and feel full sooner as food takes longer to pass through your stomach. Because it is performed using a small surgical device that your doctor passes into your stomach through your mouth, it requires no external incisions and results in no external scars on your skin. Your doctor uses a suturing tool to reduce the volume of your stomach. Typically this type of obesity surgery requires no overnight hospital stay. However, you do receive medication that puts you to sleep while your doctor performs the procedure. This type of procedure is reversible.
Making a Choice About Obesity Surgery
If your health care professional recommends obesity surgery, take the time to learn about your options, ask questions, consider the pros and cons, and think carefully about whether it's the right choice for you. It's a big step — one that hundreds of thousands of people in the U.S. take each year — and should not be taken lightly. If you decide to proceed, the better prepared you are, the likelier you will be to reach your weight-management goals.
Learn more about the different types of obesity surgery procedures at the American Society for Metabolic and Bariatric Surgery (ASMBS).
Did You Know?
Obesity Surgery
- The first obesity (bariatric) surgery was performed in Spain during the 10th century.
Shared Decision-Making
You and your health care professional will work together to create a personalized treatment plan that's right for you and lets you manage your weight in a healthy way. Once you begin treatment, you and your health care professional can keep in touch to assess your progress and make any necessary treatment adjustments.
Learning you have stage 3 obesity can be frustrating. That's a normal reaction. But don't let it hold you back from considering all your treatment options. And remember that losing even 5%-10% of your body weight could improve your health and quality of life!




 DOWNLOAD
DOWNLOAD