What Is Hyperthyroidism?
Hyperthyroidism occurs when the body makes too much thyroid hormone. This disorder occurs in almost one percent of all Americans and affects women five to ten times more often than men. In its mildest form, hyperthyroidism may not cause recognizable symptoms. More often, the symptoms are discomforting, disabling or even life-threatening.
What Causes Hyperthyroidism?
- Graves’ disease: Graves’ disease (named after Irish physician Robert Graves) is an autoimmune disorder that results in thyroid enlargement and hyperthyroidism. In some patients, swelling of the muscles and other tissues around the eyes may develop, causing eye prominence, discomfort or double vision. Like other autoimmune diseases, this condition tends to affect multiple family members. It is much more common in women than in men and tends to occur in younger patients.
- Postpartum thyroiditis: 5 to 10 percent of women develop mild to moderate hyperthyroidism within several months of giving birth. Hyperthyroidism in this condition usually lasts for one to two months. It is often followed by several months of hypothyroidism, but most women will eventually recover normal thyroid function. In some cases, however, the thyroid gland does not heal, so the hypothyroidism becomes permanent and requires lifelong thyroid hormone replacement. This condition may occur again with subsequent pregnancies.
- Silent thyroiditis: Transient (temporary) hyperthyroidism can be caused by silent thyroiditis, a condition which appears to be the same as postpartum thyroiditis but is not related to pregnancy. It is not accompanied by a painful thyroid gland.
- Subacute thyroiditis: This condition may follow a viral infection and is characterized by painful thyroid gland enlargement and inflammation, which results in the release of large amounts of thyroid hormones into the blood. Fortunately, this condition usually resolves naturally, with the thyroid healing itself over several months, but a period of hypothyroidism may occur before recovery.
- Toxic multinodular goiter: Multiple nodules in the thyroid can produce excessive thyroid hormone, causing hyperthyroidism. Typically diagnosed in patients over the age of 50, this disorder is more likely to affect heart rhythm. In many cases, the person has had the goiter for many years before it becomes overactive.
- Toxic nodule: A single nodule or lump in the thyroid can also produce more thyroid hormone than the body requires and lead to hyperthyroidism.
- Excessive iodine ingestion: Various sources of high iodine concentrations, such as kelp tablets, some cough medicines, amiodarone (Cordarone, Pacerone – medications used to treat certain problems with heart rhythms) and x-ray dyes may occasionally cause hyperthyroidism in patients with thyroid nodules.
- Overmedication with thyroid hormone: Patients who receive excessive thyroxine replacement treatment can develop hyperthyroidism. They should have their thyroid hormone dosage evaluated by a physician at least once each year and should never give themselves “extra” doses.
What Are Common Symptoms of Hyperthyroidism?
When hyperthyroidism develops, a goiter (enlargement of the thyroid) is often present. It also is associated with some or many of the following symptoms:
- Fast heart rate, often more than 100 beats per minute
- Becoming anxious, irritable, argumentative
- Trembling hands
- Weight loss, despite eating the same amount or even more than usual
- Intolerance of warm temperatures and increased likelihood to perspire
- Hair loss
- Tendency of fingernails to separate from the nail bed
- Muscle weakness, especially of the upper arms and thighs
- Loose and frequent bowel movements
- Smooth skin
- Change in menstrual pattern
- Increased likelihood for miscarriage
- Prominent "stare" of the eyes
- Protrusion of the eyes, with or without double vision (in patients with Graves’ disease)
- Irregular heart rhythm, especially in patients older than 60 years of age
- Accelerated loss of calcium from bones, which increases the risk of osteoporosis and fractures
How Is Hyperthyroidism Diagnosed?
A trained physician can identify characteristic symptoms and physical signs of the disease. Tests can be used to confirm the diagnosis and to determine the cause.
To diagnose and treat hyperthyroidism, a primary care physician will likely work with an endocrinologist, a specially trained doctor who is qualified to diagnose and treat hormone-related conditions, including diseases related to the thyroid gland.
Find endocrine care in your area.
What Tests Are Used to Help Determine Hyperthyroidism?
- TSH (thyroid-stimulating hormone or thyrotropin) test: A low TSH level in the blood is the most accurate indicator of hyperthyroidism. The body shuts off production of this pituitary hormone when the thyroid gland even slightly overproduces thyroid hormone. If the TSH level is low, it is very important to also check thyroid hormone levels to confirm the diagnosis of hyperthyroidism.
- Estimates of free thyroxine (T4) and free triiodothyronine (T3): This measures the level of active thyroid hormones in the blood. When hyperthyroidism develops, free T3 and free T4 levels rise (although they may still fall within the normal range for the general population) and are often considerably high.
- TSI (thyroid-stimulating immunoglobulin or TRAb (thyrotropin receptor antibodies): antibodies often found in the blood when Graves’ disease is the cause of hyperthyroidism.
- Radioactive iodine uptake (RAIU): a measurement of how much iodine the thyroid gland can collect, and thyroid scan, which shows how the iodine is distributed throughout the thyroid gland. This information can be useful in determining the cause of hyperthyroidism and, ultimately, its treatment.
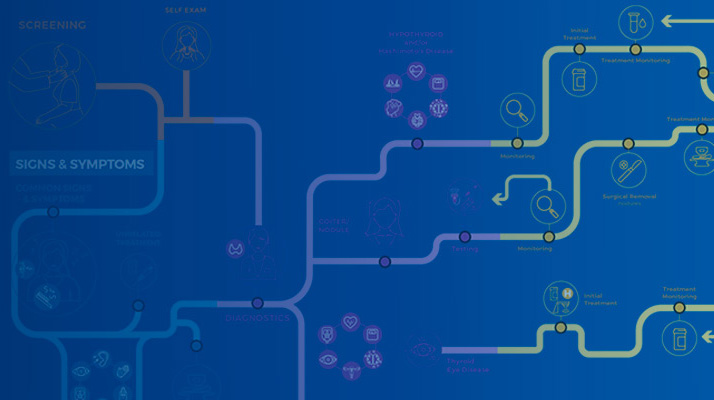
Visit our Journey for Patients with Thyroid Disease to learn more about hyperthyroidism diagnosis.
Learn More
How Is Hyperthyroidism Treated?
- Anti-thyroid medications: Two drugs are available for treating hyperthyroidism: propylthiouracil (PTU) and methimazole (Tapazole). Methimazole is usually preferred because PTU can rarely cause fatal liver damage. These medications control hyperthyroidism by slowing thyroid hormone production. They may take several months to normalize thyroid hormone levels.
- Some patients experience a remission of hyperthyroidism after treatment with these drugs, but the remission is frequently only temporary.
- Anti-thyroid drugs may cause an allergic reaction, such as a rash or hives, in about five percent of patients who use them. Also, in rare cases, the drugs may increase susceptibility to infection.
- Radioactive iodine treatment: This is generally considered the treatment of choice for hyperthyroidism cases caused by overproduction of thyroid hormone. Radioactive iodine is usually taken orally. It enters the thyroid cells from the bloodstream and gradually destroys them. Results are usually seen within 3-6 months.
- It is not possible to eliminate a precise amount of the diseased thyroid gland, since radioiodine eventually damages all thyroid cells. Therefore, most endocrinologists strive to destroy the diseased thyroid gland with a single dose of radioiodine.
- This results in the intentional development of an underactive thyroid (hypothyroidism), which is easily corrected by lifelong thyroid hormone replacement therapy.
- Surgical removal of the thyroid: In rare circumstances, operating to remove most of the thyroid gland is recommended. For example, surgery may be the best option for a pregnant woman with severe uncontrolled disease in whom radioiodine would not be safe for the baby.
- Surgery usually leads to hypothyroidism, which is treated by lifelong thyroid hormone replacement therapy.
- Other treatments: Beta blockers may be used temporarily to control hyperthyroid symptoms until other therapies take effect. In cases where hyperthyroidism is caused by thyroiditis or excessive ingestion of either iodine or thyroid hormone, this may be the only type of treatment required.
- Additionally, iodine drops are prescribed when hyperthyroidism is severe or prior to undergoing surgery for Graves’ disease.
Visit our Journey for Patients with Thyroid Disease to learn more about hyperthyroidism treatment options.
Learn More